Latest News Update 20.3
October 26, 2022
Dear Patients
This is our latest news update following on from our last one in July. Previous updates issued throughout the course of the pandemic can be found here.
We have lost several GPs recently, leading to increased workload and stress for the whole team and some difficulties for our patients. We therefore think it timely to speak openly and honestly about the GP workforce crisis continuing to unfold nationally.
It's a long read, but hopefully informative, so if you are interested, make yourself a drink, put your feet up and please take your time.
COVID CASES RISING
As of last week, the latest estimates from the Office for National Statistics (ONS) suggest one in 37 people in the UK has coronavirus, a rise from one in 50 the week before with a notable rise in older people.
We urge people to continue to take care.
Current guidance indicates that any patient attending with respiratory or viral symptoms, or who has not spoken to a clinician prior to attending, will be required to wear a face covering that covers their nose and mouth as part of ongoing infection, prevention and control measures. In order to protect our staff and vulnerable patients, if you actually have covid, please do not enter the building - if you need attention, always ring us first.
GOV: Next steps on infection prevention and control What to do if covid positive What to do if unwell with covidHopefully we will weather this winter with the help of the autumn 2022 covid booster campaign. Accordingly we have updated our covid vaccine information page to provide the latest details.
The following patients will be eligible for an autumn booster: housebound, care home residents, care home workers, frontline health and social care workers, pregnant, those aged 50 years and over, those with at-risk medical conditions and household contacts of an immunocompromised individual.
Please see our covid vacc page for details on how to book your covid jab:
IGS: Covid vaccPlease note that for logistical reasons, the surgery is not providing joint covid and flu jabs. Covid jabs are provided at the Church Farm Hub (where Ivy Grove Surgery and Jessop Medical Practice are based). Flu jabs are provided to our own patients by the team at Ivy Grove Surgery.
IGS: Flu vaccWE ARE SHORT OF GPs
Things remain difficult as ever at the surgery, by the time you read this another doctor will have left the surgery. This time it is Dr Irfan, who is relocating to the Middle East with his family, with Dr Smith already having relocated down south to be closer to family.
In total we have now lost 17 sessions of GP time which equates to anything from 60 to 80 hours of appointments lost. We have attempted to meet the shortfall with locums however these are not always available and long-term, are not a viable and sustainable solution.
We have now been advertising three GP posts in a variety of forums, but have so far attracted very little interest in six months. This does represent a massive change from normal circumstances where we usually get a number of suitable applicants. This indicates the situation is not 'normal' and also it is not unique to our surgery as locally other practices are facing similar struggles; it is an indication of the crisis in General Practice that is being experienced nationally.
IGS: JobsConsequently our GP appointment capacity has been affected as we do our best to provide a safe service to our patients, whilst at the same time, trying to safeguard the health and wellbeing of our remaining GPs and team members. If we are full for the day, you may be asked to attend another service, or ring back another day, try self-care or use the resources on our website as detailed below.
OPTIONS IF WE ARE FULL
If we are full that doesn't mean you should just sit at home and suffer. There are options available to everyone in order to start to get the help that you need.
ATTEND ANOTHER SERVICE
IGS: Self-refer IGS: Urgent treatment care for same day care NHS: When to visit an urgent treatment centre IGS: 999 ambulance in a life-threatening emergency IGS: Accident and emergency Ring 111 for adviceGET TRUSTED MEDICAL INFORMATION
NHS: A-Z of conditions Patient.info health topicsUSE AN ONLINE SERVICE TO FIND OUT WHAT TO DO
NHS 111 online triage service Patient.info symptom checker IGS: Symptom checker IGS: Self-care IGS: Mental health IGS: GP TeamREAD AN INFO LEAFLET ABOUT YOUR CONDITION
IGS: Downloads NTW self-help leaflets on mental health conditionsGP WORKFORCE ARTICLE
If you wish to share this article, or need to come back to it at a later date, use the shortcut ivy.gs/gp-crisis
You can also download the article for offline reading .
INTRODUCTION
What follows now is an extended piece regarding the GP workforce, which references the external political situation that General Practice and the NHS find themselves in. You will have heard the almost daily news stories on the state of the NHS, its hospitals, the ambulance service and our own service, General Practice and in particular GPs.
The NHS was and is a political construct, the nation’s beloved social enterprise, and General Practice itself is synonymous with the NHS, since its inception. Therefore the NHS, and in particular General Practice and GPs are never free from political interference.
We have no doubt that it is this external political interference over the decades, both through deliberate action and neglectful inaction, that is now finally bringing the NHS and in particular, General Practice, to its knees. As we have seen recently, it is perfectly possible for any government, through a series of bad decisions, to completely mismanage something and bring the country crashing down, so General Practice is no different.
We make absolutely no excuses for bringing this to the attention of our patients. There is much more behind the simple attention-grabbing headlines about work-shy GPs that demands thorough explanation to unravel. The complex situation, around demand, workload and why the service is short of GPs and in need of help, needs clarifying.
Hearing all this might be unwelcome news to some, but at Ivy Grove, we have never shied away from telling people the truth. Even with the loss of three GPs recently, the doctors at Ivy Grove still have over 110 years of experience in the NHS between them. We do know a bit about General Practice and the NHS, what is going on and what needs to happen to help it out of a dire situation.
What we can do and can't do in practice is subject to so much external influence that ultimately it can affect our ability to provide safe practice. As responsible doctors, we have an overriding duty to act in order to maintain the safety of our patients and that of our own wellbeing. Part of this involves informing you of what is going on behind the scenes so that you know why things are the way they are.
But at the end of the day, if all you want is an appointment with the GP and you're not interested in why you then can’t get one, feel free to skip any or all sections. Otherwise, please read on.
ARTICLE SUMMARY
It might seem daunting to read the whole thing, but we do recommend it, when you have the time, or you can just bookmark it for later reading, it will still be here on the website for you. If you don't want to read the whole article, please find the summary below:
WRITTEN SUMMARY
1
NOT ENOUGH GPs Official NHS/government figures show unequivocally that there are fewer GPs dealing with more and more work. There are simply not enough GPs to meet the demands of the service. This is leading to increased stress and risk of burnout in remaining staff, and reduced patient satisfaction with the service.
2
IMPROVE THE JOB We need more GPs. Whilst other workers are more than welcome to join the GP team to help meet demand, no amount of other workers will ever replace a GP. No amount of proclaiming or promising more GPs without actual efforts towards making the job more rewarding and more manageable will work, because GPs will continue to leave the service faster than they can be recruited.
3
HAVE A PROPER PLAN Rather than pandering to public misconception and the vicious need for scapegoating, the government needs to admit that there is a crisis in General Practice, listen to the profession and its own advisors and enact viable suggestions for change that will help to make General Practice sustainable for the future. There needs to be immediate short-term changes to relieve pressure instantly, but also longer-term planning to meet the challenges placed upon the service.
4
EDUCATE THE PUBLIC Whatever happens, General Practice will still ultimately be a limited resource, therefore there needs to be a frank and honest debate with the public on what is demanded of the service and that this needs to be balanced against the resources available, and this should always be against a background of sustained public health programmes and continued education.
5
IF GENERAL PRACTICE FAILS... If nothing real and positive is done about General Practice, the safety of all patients and of all the staff in GP teams will be at risk. Consequently, if General Practice fails, then without a doubt, the rest of the NHS will follow very shortly after. This will be to the detriment of all of us, as we are all patients.
VISUAL SUMMARY
For a quick visual summary of some of the points raised in the following article, please see the following videos. Although these videos were made five years ago, they are still very relevant today.
GP WORKFORCE CRISIS
We at Ivy Grove are not alone in struggling to recruit GPs. This is a problem that is affecting other local practices and also nationally. GP forums are full of unanswered job adverts. Staff are being poached from one practice to another in unsustainable bidding wars. Practices are closing around the country due to lack of staffing.
As shown by the latest GP practice workforce data, from the government’s own figures, as of August 2022 there are now 1,850 fewer fully qualified full-time GPs compared to September 2015. This is at a time when in August 2022, GPs delivered a staggering 3 million more appointments than in August 2019, meaning that surgeries are now managing the levels of demand they used to see in a pre-pandemic winter in the middle of summer.
NHSE: General Practice Workforce, 31 August 2022 NHSE: Appointments in General Practice, August 2022We know you are struggling to get in to see us, or to speak to us, that’s because there are fewer of us, and we are doing more, proven by the government’s own figures. You are all experiencing the other side of the difficulties that we and our staff face in the surgery every single day. Therefore it is utterly demoralising and puzzling in equal measure to hear that the new health secretary has recently stated that there is no crisis in General Practice!
PULSE: Health secretary claims GP numbers are ‘stable’It is also equally interesting that on the very day that the nuclear threat from a global superpower became a plausible possibility and interest rates went up yet again signalling a potential recession, these two very newsworthy items were superseded on the front pages by yet more GP bashing in the form of promises from government to force GPs see you face-to-face within two weeks, because we’re lazy and on the golf course and/or have been hiding behind our desks, not seeing anybody, in fact doing nothing much at all these last three years!
BMA: Health Secretary’s new plan brings us closer to the demise of general practiceAside from the health secretary adding yet another target to those that GPs already have to work to, quite how this promise would be implemented remains to be seen given that there appears to be no extra resources or plans to bring more GPs into the service, or indeed, to retain those GPs who are already in the service.
Seeing a patient within two weeks is on par with the time period set for a patient to be seen at the hospital if they have been referred by their GP due to suspected cancer, as some of you will know, having been through that experience. If we are now saying that every patient must be offered a face-to-face appointment within two weeks with the same clinical priority as a potential cancer patient, then the question arises, what other important work do we drop in order to meet this requirement?
UPDATE NOV 3, 2022: In an display of blatant one-upmanship and equally startling ignorance, the Lib Dems have decided to do one better than the Tories and have stated that they would force GPs to see every patient within a week, again with no mention of any plan or additional resources to meet such a pledge.
And to show we're not siding with just one or other party here, we're equally dismayed by Labour's pledge of September, where they stated they would force GPs to offer everyone face-to-face appointments, again ignoring what is happening on the ground and the changes made since the pandemic.
Notice the word choice from all parties. All political parties here are wilfully ignorant of the issues around General Practice, and rather than tackle the root causes of the crisis, all parties are pandering to public expectation, without providing any sound plan to meet such expectations.
Targets And Safety - By Jeremy HuntIt's a turn up for the books when you find yourself agreeing with the comments of a former health secretary, Jeremy Hunt* in the above blog:
*Although this same health secretary resided over unwelcome impositions to the GP contract (which I personally wrote to him about ) and also over the junior doctor 7 day working week crisis, as well as many other issues, all to which he was fairly tone deaf whilst in office†
†After several years of rhetoric and espousing much support for the NHS and NHS workers since his time as health secretary, let’s hope that Jeremy Hunt, now chancellor, will actually put his money where his mouth is and realise that support into genuine tangible resources and much needed help for NHS staff, however we're not going to hold our breath, because we'd probably suffocate
The former health secretary Jeremy Hunt, now Chancellor of the Exchequer, also led the House of Commons Health and Social Care Committee which has only just published a new report into General Practice:
HSCSC: The future of general practiceEssentially it issued stark warnings of a demoralised profession, with GPs facing burnout from working in a ‘systemically toxic environment’, with unsustainable workloads, managing intensely complex cases at speed with fear over reprisals.
Here are some more notable quotes from the extensive report (our italics):
BMA: Recommendations in HSCC report must be acted on to ease pressures in general practice
Ultimately what we need in General Practice is for the government to take urgent action on making the job more attractive, so that there are actually more doctors wanting to become GPs and so that there are fewer of us wanting to leave the profession. We are not hopeful that the government will listen and take the necessary steps to improve General Practice. The following is a detailed breakdown of what is required.
WE NEED MORE GPs
From a previous newsletter you will be familiar with the additional roles that have been promoted as part of the GP team. Notwithstanding the difficulties in recruitment, ultimately, whilst more members of the GP team are useful, the rigid government rules regarding employing extra staff specifically excludes doctors and nurses, the very team members that we are so desperately short of. You will notice the soundbites coming out of government ostensibly helping to relieve the pressure on GPs and their teams, but always falling short of providing more GPs, more nurses, more receptionists and admin staff, which are actually the sort of staff we need.
So for instance, in order to relieve pressure on GPs, the health secretary has declared that we are to have ‘pharmacists prescribe antibiotics’. So we have her on the one hand, citing her own experience of dishing out leftover prescription medication to her friends as 'evidence' that this would be appropriate, and on the other hand, her comments lay bare the common public misconception that all GPs ever do is prescribe antibiotics (and refer people to hospital and write sick notes). And all the while being completely ignorant of the real issues behind antibiotics, such as most upper respiratory illness presenting to general practice is viral, the risks of inappropriate use of antibiotics and of bacterial resistance and the potential to harm patients and importantly, also ignoring the real issues and causes behind GP workload.
In another example, the government has said that to help with winter pressures in General Practice, it, planned to bring in 1,000 link workers, however if you do some quick maths this equates to roughly 1/8 of a person per practice, which is of course, no use whatsoever. It's quite literally, just giving us a 'hand'!
And yet another example, as part of the uncosted and unresourced ‘plan’ to make GPs see patients face-to-face within two weeks, the government announced, ‘an additional 31,000 telephone lines available for GP practices’, this would equate to around 3 or 4 extra lines per practice, but obviously there is no mention of any extra reception staff to answer these incoming calls or any GPs or practice nurses to deal with the resulting appointments.
No amount of frivolous tinkering around the edges of the situation will ultimately resolve the problem. At all.
It has previously been indicated that the NHS wishes to aspire to the unassailable safety processes of the airline industry. Well, let’s take the potential analogy further: in the same way that it is only pilots who are able to get the plane off the ground, no amount of extra check-in staff or baggage handlers, though they are of course, vitally important to the process, will get you to your destination. You need pilots. You need pilots who are happy, well-rested, motivated and above all, working safely, to get you to where you need to go. The NHS needs General Practice. General Practice needs GPs. End of.
HEALTH: A quarter of GP and general practice nursing posts could be vacant in 10 yearsSo, how do we get more GPs? Please read on.
HOW TO GET MORE GPs PART I
The government's recently published 'Our Plan for Patients' seeks to address four main areas of concern in the NHS at the moment, one of which is doctors (GPs). But it is simply just a series of aspirations and it is rather short of any actual plans. See for yourself:
GOV: Our Plan for PatientsWe touched on some of what is immediately required to help the situation in a previous newsletter:
IGS: Additional roles in the GP teamBut let's flesh things out further with some proper explanation.
A 10-POINT PLAN FOR SHORT-TERM GAIN
Any actions that do not immediately relieve the pressure in General Practice such as some of those suggested below will not make any difference. The government enjoys spinning the same old message as mentioned previously, of more GPs promised, more in training, more medical students, with little regard for the fact that it takes 10 years or more to train a GP, from enthusiastic student to a fully qualified doctor. Therefore the mention of more GPs is never going to be a quick solution and will not have any immediate impact upon current GP numbers.
Rather than just moan about how hard the job is, or how short-staffed we are, how about we actually come up with some positive ideas to improve the situation? Any of these suggestions, which could be achieved if the will was there, would start to make a real difference to General Practice. Here are some real solutions:
1
ALLOW PRACTICES FLEXIBILITY The rules regarding additional roles in the GP team need to be immediately relaxed so that practices can directly employ GPs and practice nurses to relieve the workload pressure, or if the permanent staff are not available, then locum doctors and bank nurses; there needs to be enough flexibility in the system to allow networks of practices to hire who they want, according to the needs of their local population, and not according to the restrictive regulations and unrealistic expectations of those in isolated ivory towers.
2
ATTRACT MORE GPs The job of a GP needs to be made more attractive immediately. There are many ways to achieve this. This could be via a significant reduction in or the complete abolishment of the number of targets, a slowing of the incessant pace of change or the relaxation of existing targets to simply allow some breathing space [in order to obtain full payment for some targets in the GP contract, GPs and their teams must achieve a ridiculous 97% success rate, and in the childhood vaccination targets, there is no consideration that parents might decline, leading to practices missing out on the target completely].
There should be a light-touch approach to the contract and easing of burdensome over-regulation, micro-management and scrutiny and a return to actually trusting professionals and leaving them alone to do their jobs. There should be cutting the amount of red-tape and administration required to simply do the job [some of the emergency changes brought about as a result of the pandemic truly did make a difference to the workload of a GP, but quite predictably, tedious and completely unnecessary administration has insidiously crept back into the job, well, just because].
3
END CALLS FOR GPs TO DO MORE There should be a conscious effort to reduce demand on the GP service, by not overloading it with things that it is not in a position to perform; there should be an immediate freeze on any initiative, press release, soundbite, headline, article, development, research piece, study or any other public announcement declaring that ‘GPs should…’ or ‘GPs are best placed to…’, especially where such pronouncements are made without any mention of resources, funding or even a plan.
GPs are more than busy enough with their day-to-day work to be the entire back-stop and risk-sink for the whole of society. We could fill all the newsletters for the next 10 years dissecting the multitude of hare-brained schemes dreamt up by simply everyone on what a GP should do to resolve whatever perceived need there happens to be in society. The most recent and frankly one of the most ridiculous was this new government’s plan for GPs to prescribe people money off their energy bills [seriously, it’s not a joke, please look it up].
4
ACTIVELY RELIEVE DEMAND As well as not adding to the demand as mentioned above, there needs to be a proper focus on actively relieving the demand on GP teams; you could start by educating the public, by encouraging self-care, by actively directing patients to the multitude of other workers in the NHS who are geared up to take direct referrals from patients, by making such choices absolutely clear to everyone, who to see and when, by abandoning the standard ‘see your GP’ mantra for everything that has caused GP services to be completely overwhelmed over the last few decades, and change it to ‘contact your GP team’, or even, more appropriately ‘who do you need today?’
As part of this process, there needs to be immediate moves to limit inappropriate transfer of work from other parts of the health service onto GPs, what GPs affectionately call 'dumping'. Many of the demands placed on General Practice arise not from patients themselves, but from other workers, again following the decades-old mantra of 'see your GP' or 'speak to your GP'. And GPs are bombarded daily with requests by other workers to prescribe this or that, to chase a result, to write a sick note, when the worker making that request could actually and easily have done the task themselves, often with the benefit of the patient actually there in front of them!
5
RETAIN GPs AND PARTNERSHIPS As well as the financial incentives that encourage trainees to work in deprived areas and doctors to join GP partnerships, there needs to be equivalent inducements to retain longstanding and experienced clinicians in the system, otherwise such GPs will continue to leave the profession because quite simply they have had enough of the punitive arrangements that penalise hard work and long service in the NHS.
Related to this, the partnership model of General Practice needs to be cherished and actively invested in as it is the key to responsiveness, innovation, commitment, efficiency and a deep sense of ownership in making a real difference for patients - it has without a doubt stood the test of time and been the only constant against a plethora of changes within the NHS. There needs to be a move away from actively damaging the partnership model, the buying out of partnerships and the privatising of GP surgeries in favour of big business out to make a quick profit from a system that is already as lean as it could possibly be.
6
BE HONEST WITH THE PUBLIC There needs to be a frank and honest discussion with the public on what they truly want from what is ultimately a resource-limited service and if what is desired is an all-you-can-eat, 12 hours a day, 7 days a week or indeed 24 hours a day service immediately assessing and managing any complaint, regardless of clinical urgency, which is fine by the way, if that’s what you want, but then the question must be how might that be developed and resourced properly, because it is clearly impossible within the current constraints of staffing and resources. NHS England and the government, please note, no matter how hard you shout out about it, no matter how noble your aspiration, no matter how much you wish to appease public anger, or meet public expectation, you cannot make a unicorn out of a donkey and a bit of papier-mâché.
7
ENSURE SAFE WORKING And if no resources are forthcoming, then the questions become: what is going to be dropped to enable GPs and their teams to practice safely in the interests of their patients, their staff and their own health; what limits to consultations and workloads are going to be made to enable safe working; what crucial or urgent work is to be prioritised to keep patients from harm; what emergency procedures are put in place to protect GP and their staff from suffering burnout? Because if there are no staff, then that means no patients are being dealt with.
8
CHERISH THE GP SERVICE But if there is actually a thoughtful response that health services and its workforce should be valued and treated with respect, in order to preserve our beloved health service for future generations, for our own old age, for our children and grandchildren, then there should be public recognition that it is actually a limited resource, because as it stands at the moment, the only (impossible) mission that is bandied around seems to be access, access, and more access, and specifically GP access, regardless of priority.
And as with all things in life, the more available and easily accessible something is, the more that commodity is devalued. It ceases to become precious, to be valued, to be cherished. General Practice may well be the jewel in the crown of the NHS, but the public definitely don’t consider it to be a diamond. Your GP is already the most accessible professional in the whole of society – you would not be able to speak to or see any equivalently qualified professional with the same ease as you can with your GP [yes, we are aware that's difficult to do at the moment, but the point stands].
9
END GP BASHING Towards the end of our 10 point plan, but actually very important, there needs to be an end to the almost daily GP bashing in the press, in social media, on talk shows, on TV, in anonymous and unaccountable reviews, all of which lends strength to the belief that it is all actually part of a deliberate agenda of attack against GPs and their teams.
It's a curious thing, that in British society, of all the workers who actually do have the potential to make a real difference to your life, that the humble General Practitioner, quietly working in the background, seeing a tenth of the population every single week, to make those differences, is single-handedly, the most vilified member of society. Later on in this article we discuss this:
What the public think of GPsEven where issues are patently nothing to do with GPs, some irresponsible elements in the press will find ways to skew the perspective and somehow blame GPs for the problem.
Constantly denigrating someone does have a negative effect. It saps their energy, their heart and their soul. It increases their stress and anxiety. In domestic situations this would be classed as abusive and would need to stop and action taken against the abuser. Stopping the abuse would help to improve the wellbeing of already utterly demoralised GP teams and perhaps make them feel that their job is actually a worthwhile enterprise and making a difference.
We're not talking about filling the press with positive articles about GPs or their teams at all, by the way. That is not needed at all - although it is good for the soul to be spontaneously praised - the reason for our existence is actually not to please others and we will carry on doing what we need to do for our patients regardless of that. All we kindly ask for is an end to the constant GP bashing.
10
ALLOW RESOURCES TO FOLLOW THE WORK Finally, contractually, the decades-old model of General Practice needs to change radically to cope with the modern demands made upon it now. You may know from our previous messages that GPs are paid a one-off amount for managing your care for a year [this is around 50p per day]. This would only effectively pay for one or at most two consultations with the GP in one year in a normal transactional environment.
IGS: The state of general practiceYet most people consult with their GP much more than twice a year. The surgery does not get any more funding for seeing you more. You could visit 100 times a year and they still wouldn’t get a penny more funding. You can see how this puts strain on the service. It’s like paying a supermarket a single one-off fee and getting as many groceries as you like whenever you like – it simply wouldn’t work – you’d see empty shelves pretty much all the time before the supermarket closed for good.
It is now time to consider changing the model of how General Practice is funded, and move it in line with how other NHS services are funded, payment on a case by case basis. This would allow the resources to flow into General Practice and allow surgeries to attract, hire and retain staff to meet the growing demands of the population. [It's interesting that the initiatives promoted by NHS England to facilitate the provision of services by workers other than a GP are paid for on a case-by-case basis - there seems to be recognition that funding must follow the work, but a distinct refusal to consider the same for General Practice itself.]
But if you don't wish to move to a case-by-case basis of funding, and wish to stick with the block contract, then that contract must have capacity limits placed upon it in order to maintain safe working.
HOW TO GET MORE GPs PART II
A 5-POINT PLAN FOR LONGER-TERM CHANGE
Rather than just repeatedly spouting that more GPs are in training, how about thinking properly, longer-term, so that even with new GPs available, General Practice remains sustainable. Here are five things that could be done to start to make a difference to our society in the medium to longer-term as future GPs go through the system:
1
RETURN RESPONSIBILITY FOR HEALTH We need to educate our children and their parents and indeed prospective parents on health, on the expression and regulation of feelings and emotions, on an awareness of the body and mind and what it does and what to do when it doesn’t do what you want or when it goes wrong.
We’re not talking a biology degree by any means, just an increased sense of understanding, that needs to be an active part of the curriculum throughout pre-school, school and college and as part of university courses. There needs to be a return to a degree of ownership of one’s health and wellbeing and an acceptance of some responsibility for taking appropriate action to help oneself and to seek appropriate advice when it becomes necessary. It will probably take a generation or two to work properly, but it will be worthwhile doing.
The following maxim is a good place to start: Your health is my concern but your responsibility
2
EDUCATE THE PUBLIC The education of young and receptive minds as described above cannot be done in isolation from education of the masses, therefore there needs to be a massive public health campaign around health education – we know that adverts telling people to attend health services with this or that symptom are more successful than those that tell people not to do something (like smoking or drinking too much alcohol). We know that adverts telling people such and such a service is available are more successful than those that tell people not to use the service and instead to treat or help themselves with this or that symptom.
But considering that there has been no sustained programme on educating the public on looking after themselves, on what to look out for, and on when to consult health services (other than a GP), it would be good to start doing so. As a practice, we know sustained patient education from a motivated team and a receptive patient population does work. It has led to significant changes in how we practise, so we know that it is achievable.
3
INVEST IN SOCIAL CARE The precarious path that exists between health and illness is very often social in nature – there is increasing recognition of this with the expansion of additional roles in the GP team, such as the social prescriber, the care co-ordinator, the community matron, the health and wellbeing coach. However there has not been a correction of the significant and deliberate underfunding of social care and the active cutting of community services, and we still do not see resources follow transfer into the community where it is most required.
As a result many encounters we see in General Practice have a significant social context that must also be tackled if the patient is to return to health or a state of manageable health. And it is not only General Practice that is impacted by this; beds are routinely blocked in hospital due to lack of social care support in the community – health and social care should go hand in hand, but there is still an overwhelming focus on medical access, and negligible focus on social access.
4
IMPROVE POPULATION RESILIENCE There is always much talk of doing what is necessary to increase the resilience of healthcare staff so that they can cope with the demands and stresses of the frontline. We feel this is like teaching someone how to take a beating so that they can tolerate even more beatings to come and be OK with it. It is categorically not OK. Even if increasing resilience was actually a feasible response to the situation, there has never been any balance in the equation, nor any calls to improve the resilience of the public, or the population at large.
Again there needs to be public education programmes on managing one’s health and minor self-limiting illness, on how long simple conditions last when left to the body’s own recovery mechanisms, that the body is not a machine, nor is it meant to be perfect, that things do go wrong, but equally that many things do get better by themselves, that worry drives more worry which in turn drives sickness, that common things are common and rare things are rare, that there are things that are less concerning, that there are things that could be worrying.
Of course there is the concern that with being or becoming more tolerant, or stoic, there would be a risk of missing or putting up with serious disease, so people would come to harm, but we are not suggesting that people tolerate symptoms that could be serious; we are saying that people should be educated on the wide range of 'normality', and we suggest that there is a greater risk of missing serious disease if the service is overwhelmed by undue concern for symptoms that are not at all serious.
By managing expectation and concern, by increasing the resilience of the public at large, there should be more than enough capacity for General Practice to attend to those who truly need to speak to or see a doctor; so that people do not come to harm; so that your GP can treat patients such as those with red flags of potential cancer, those whose symptoms indicate serious ill-health, those at severe risk from physical or psychological conditions.
IGS: Poorly patient IGS: Cancer red flags5
RECOGNISE THE GP TEAM There has been much focus on GPs, not just in this plan, but everywhere. But the other workers in the GP team are equally important. We know there are moves towards increasing the range of other workers in the GP team but actually much of the solution lies closer to home.
There should be a renewed focus on practice nurses, on GP receptionists, on GP admin staff, without whom GP surgeries would collapse overnight. The fact that government plans for practices and networks of practices and additional roles for practices excludes these essential workers indicates how short-sighted those initiatives are.
It takes a trained receptionist to answer your call, to listen and react to your request and book you or signpost you appropriately; it takes a qualified nurse to manage your chronic disease, to perform your heart tracing or dressing, to assist the doctor with your minor operation; it takes an admin worker to chase up your test result, to book your hospital appointment, to type out your referral letter. All of these form an absolutely essential part of providing care to each and every patient, a lot of which is done in the background, and which is not counted, but it still counts.
Longer-term, in any investment plan for General Practice, there should be a focus on providing for and supporting such staff, to make their working lives rewarding too, with recognised training and qualifications, and career progression. Whenever the government makes those promises of more GPs being on the way, why not also make the promise of more practice nurses on the way, and more GP receptionists and admin staff on the way? The promises might well be empty, but at least it would be a start to improved recognition of the traditional GP team.
There is also a need to include GP staff in any public campaign to promote zero tolerance against abuse; the shortage of GPs is felt by all GP receptionists most acutely, because they bear the brunt of public anger when faced with the consequent lack of appointments. They should not have to tolerate this.
But don't just take it from us: read the honest view from one of our receptionists later on in this article:
A message from reception Zero tolerance videoBUT NO-ONE LISTENS
Having said all the above, and suggested workable short-term plans and longer-term changes, will anyone listen? We're not hopeful. Rather than actually listen to the profession, the government continues to ignore that there is a crisis and instead continues to pander to public perception of GPs. Even in its 'Our Plan for Patients' the government titles the section on GPs with 'Primary care: meeting public expectations'. It needs to be pointed out that meeting public expectations is how you win votes, not how you fix General Practice.
If you ever want to know what the public are thinking about any topic, just type half a sentence into Google and see what the predictive engine comes up with. So if you type ‘why are GPs’ into Google, what do you get? Here’s a screenshot:
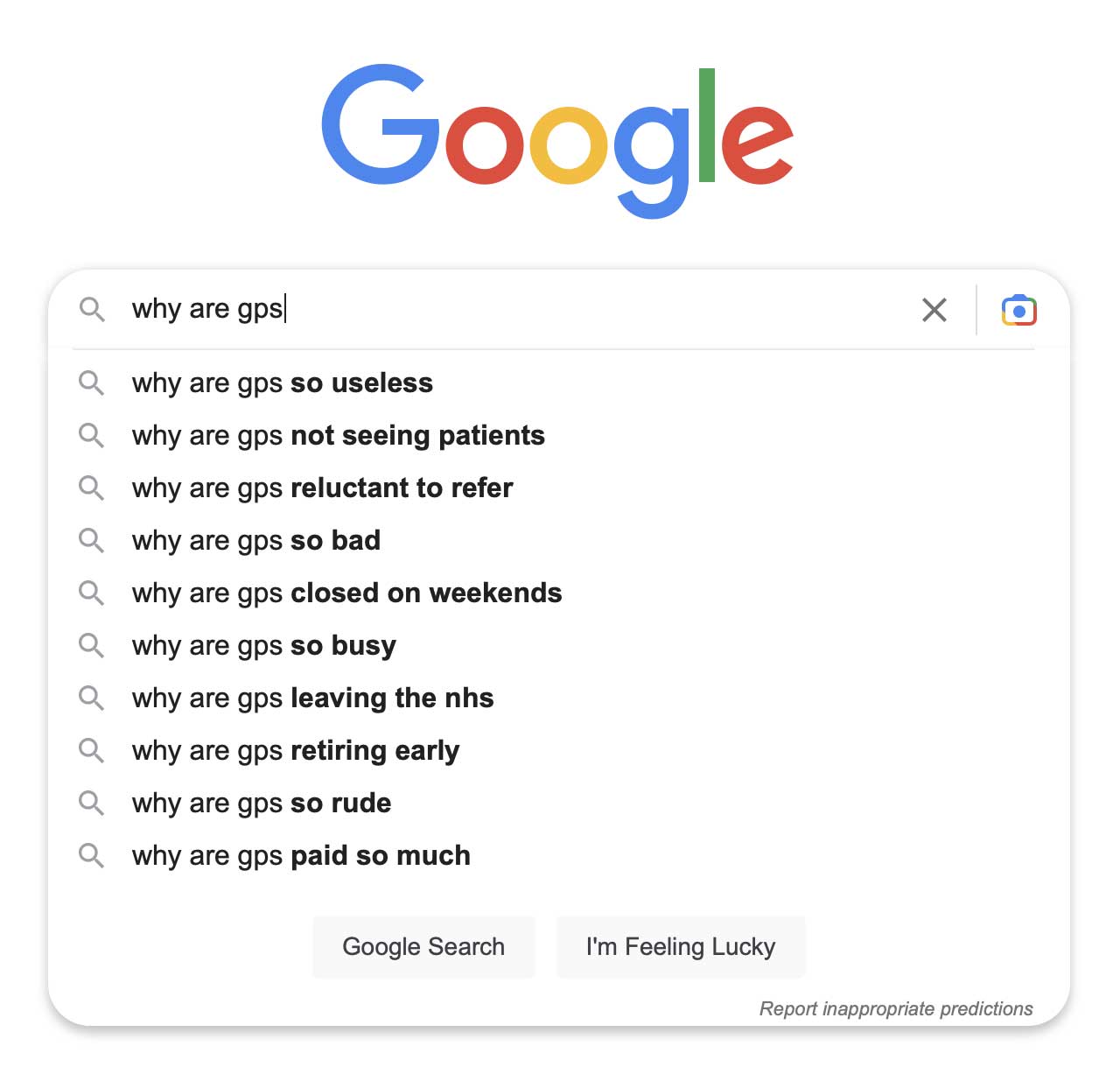
Again, as indicated in a previous newsletter, this is a yet further proof of Schrödinger’s GP. On the one hand, GPs are not seeing patients, are so useless and don’t work weekends, yet they are so busy that you can’t get an appointment. And on the other hand they are also paid so much and are so bad that they are all retiring early and leaving the NHS!
The above is just a sad reflection of the state of affairs we are currently in, as witnessed in national media and the flurry of negative one-star reviews, and confirms what has often been said, that the public hate GPs and GP surgeries in general, whilst perhaps having more positive feelings towards and maintaining good working relationships with their own individual GP [as GPs, this is what we value, it is the essence of General Practice].
A MESSAGE FROM RECEPTION
Perhaps you might be thinking having read all the above, that it is just one sad doctor’s sorry perspective. Or that they're just burnt out and having a rant against the system [for the avoidance of doubt, the author is not burnt out, far from it, and if this is a rant, then it's a comprehensive, researched and organised one]. Or perhaps you don’t believe a word of the House of Commons Health and Social Care Committee's extensive 61 page report. Well, to provide another view, we now hear from one of our receptionists, the public face of the practice, behind the front desk and behind every phone call you make to the practice:
The past six or so years has seen many changes in the life of a medical receptionist. Prior to the Covid-19 years, patients would simply contact us by telephone or come into the surgery to book in for the daily 'sit and wait' clinic, we were always very busy but it was generally manageable, however since the highly successful vaccination programme and a 'return to normality' it would appear that there has been an underlying change in the way which patients consider their state of health and to the way in which they expect to be treated.
It's completely understandable having survived what has been an unprecedented couple of years but it has certainly had an effect on the workload of the receptionist and the way in which we are expected to deal with their worries and concerns. There are so many situations where a trip to the local pharmacy would be perfectly adequate but now patients generally prefer to book a chat with a doctor and in many instances insist on it!
This, of course, hasn't been helped by the shortage of GPs at Ivy Grove, although the problem is nationwide. It would appear that anyone aspiring to a career in the medical profession may well be having second thoughts which is very sad for all concerned.
The upshot is that we now have a greater number of patients asking, and more importantly expecting, to speak directly to fewer GPs and naturally becoming more and more frustrated either because telephone lines are busy or because when they do eventually get through, they are told that all available appointments have been taken.
For patients that decide to come down to the surgery at 8.00am expecting to book to see or speak to a doctor when we know in advance that this won't be possible, it is inevitable that there will be lots of very disappointed people as there are so few appointments, this leads to unwelcome confrontations only adding to the frustration; the verbal abuse being directed to the receptionist has been unacceptable for a long time and it is certainly getting worse.
Having stressed these very negative points, it is also important to point out that we do have some wonderful and kind patients who are very understanding, but something really needs to be done about the minority who abuse the frontline receptionists, we really shouldn't have to put up with it.
Although the doors and the phone lines open at 8.00am we arrive at around 7.45am to make sure that everything is ready, the computers logged on and set to go but once the calls start, that is it, the calls do not stop until 6.00pm. It is good to be busy but when it is so non-stop it is extremely tiring and draining. We also have a list of tasks and messages from doctors and nurses which may involve having to contact patients, these tasks can reach in their hundreds and so when confronted with a telephone that doesn’t stop ringing keeping up with the tasks is ever more difficult.
This is quite frankly a 'no win' situation for the receptionist and we wonder whether increasing the amount of doctors would even make a significant difference? Patients approach to the health service has changed so much that the current system is slowly becoming unworkable and change is needed sooner rather than later…
The work of a receptionist is indeed ever more difficult but I do like to believe that I am at least making some sort of a difference by helping as much as I can and when the job allows me to.
WE NEED TO STAY SAFE
We hope that this extended essay on the state of General Practice has informed you of the current situation that GPs and their teams all round the country find themselves in, but we hope you realise that we also offer some solutions to those who have the ability to make such changes. All of us are patients, all of us require GPs, now or in the future and it is therefore in all our interests to ensure that the situation improves.
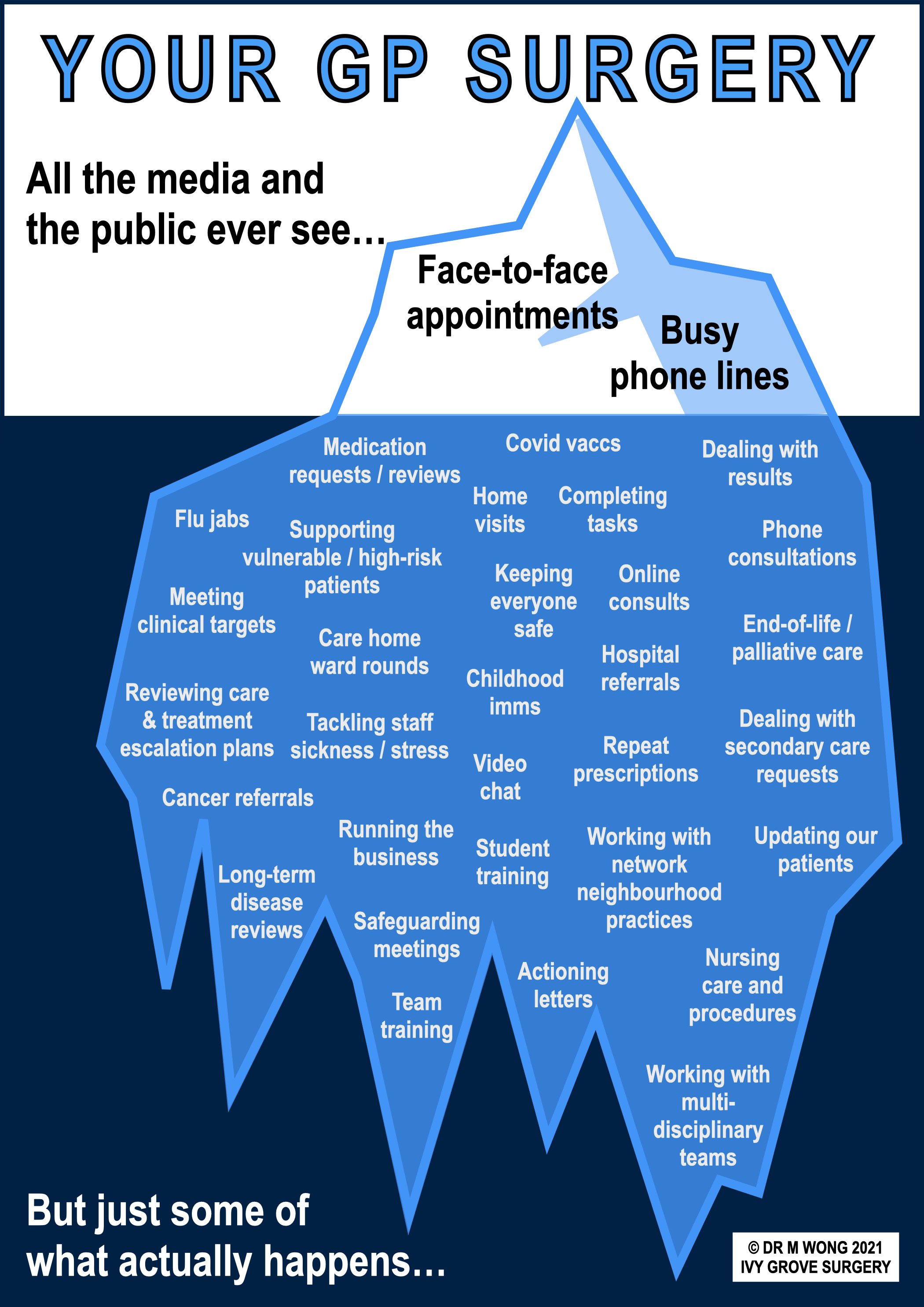
With regard to our work, all of us here in the Ivy Grove team are doing our very best in what are extremely difficult circumstances, therefore we ask that you bear with us at this time. We are dead on our feet, we are answering the phones, we are ringing you, we are calling you in, we are seeing you, we are speaking to you, we are helping you, but not only that, we are working behind the scenes doing all the things that are required to care for you (the rest of the iceberg that you can't see).
With all of this, there is only so much that we can do in the day and still be safe. As doctors we have a duty to our patients, and this duty extends to maintaining safe working practices so that we do not put the welfare of our patients or our staff at risk. At a time of unprecedented pressure and workload, and with a shrinking workforce, we will be following recognised guidance on maintaining safe working practices for our staff and our patients.
BMA: Safe working in general practice Contact your MPWe extend our thanks to all our patients for listening and for sticking with us during these testing times.
MENTAL HEALTH SUPPORT
It was World Mental Health Day on October 10, 2022, therefore it would be timely to remind all our patients of the extensive mental health resources that we have published on our website.
Throughout the pandemic we have been inundated with calls from patients of all ages expressing difficulties with their mental health. In a bid to help our patients, we have collected many resources that are available out there on one page, so that when ready, these can be referred to, in order to further support patients on their journey to recovery.
If you have a consultation with us regarding your mental health, as part of the support offered, we may signpost you to the website and also text you a series of messages reiterating the advice given and also linking to various sections of the website. This is not to bombard you with too much information, it is actually so that you can have the information ready on your mobile phone to refer to at a later date when you are ready.
VISITING THE MENTAL HEALTH SUPPORT PAGE
If you need to get to the mental health page, please use the shortcut ivy.gs/mentalhealth
IGS: Mental health supportAlternatively, click the yellow/amber button entitled ‘Mental health’ the top of the page when on a desktop, or the yellow/amber button entitled ‘Get mental health support’ on various pages of the website. Or open the menu on your mobile phone (click the three bars top right of screen), go to ‘Popular right now’ and click ‘Mental health support’.
If you are suffering with your mental health the following is a brief outline of what you can do about it.
LOOKING AFTER YOUR PHYSICAL AND MENTAL HEALTH
Please look after your physical and mental health as best you can. We realise this is very difficult in this situation but it gives you the best chances at recovery. Examples include eating a healthy diet even if you have little appetite; going to bed on time or have a regular sleep habit, even though you know it will be a struggle; keeping your mind active with interests and hobbies even though concentration is difficult; avoiding smoking or excessive alcohol even though there is temptation there; talking to friends and family even though you don’t feel like interacting; going outdoors for fresh air, exercise and sunshine to help clear the head, even though you might lack the energy, motivation or willpower.
No-one is expecting you to do all of these things all at once, but your journey to recovery starts with small choices, small steps each day. What will not help is doing nothing at all to support or improve your physical and mental wellbeing.
IGS: Stop smoking IGS: Alcohol servicesCONSIDER COUNSELLING
Please consider self-referring to free NHS counselling. Studies have shown talking therapies (with or without medication) has the best chance of successful recovery. Counselling looks at your thought processes and helps you to find answers to your condition and gives you to the tools to be able to help yourself, now and in the future.
IGS: Counselling IGS: CounsellingMEDICATION INFO
If the doctor starts you on medication, please follow their directions. Common side effects include headache, nausea, dizziness, sweating, stomach disturbances, but most people are fine, and symptoms tend to settle within a week. Please book a review appointment before you run out and never stop tablets suddenly. When stable and considering coming off, contact us and we will advise on how to do it safely..
RING THE ALWAYS AVAILABLE MENTAL HEALTH HELPLINE
If you need to talk to someone straight away any time of day or night, you can ring the Derbyshire Mental Health Helpline and Support Service on 0800 028 0077. This is a freephone service available to everyone living in Derbyshire - both children and adults. It is open 24 hours a day every day.
Mental health helpline Ring 0800 028 0077OTHER RESOURCES
It's not all talking therapy. Other help and support is available, for instance, specific information regarding younger children, older adults, dementia, sexual abuse and also leaflets on mental health issues, and other workers in the NHS, including social prescribers, our care co-ordinator team and also our health and wellbeing coach.
When on the mental health page, click the relevant tab according to age group to get to the right section:
IGS: Support for kids IGS: Support for teens IGS: Support for adults / general IGS: Support for older people / vulnerable IGS: Health and wellbeing coach IGS: Social prescriber IGS: Care co-ordinator NTW: Mental health leafletsTACKLE YOUR SLEEP DIFFICULTIES
Poor sleep or difficulties in getting off to sleep or early wakening or lying there thinking about things can be features of your condition. Lack of sleep affects our performance, decision making, thinking processes and makes us muddled and feel unwell. We therefore have a dedicated help and support section on our website for hints and tips on improving your sleep.
IGS: Sleep adviceWHAT TO DO IN A CRISIS
If you need help in a crisis or are at imminent risk of self-harm, please do seek help - you're not alone. If your or someone else’s life is in immediate danger, please call 999, or go to A&E now if your or someone else's life is at immediate risk - for example you have seriously injured yourself or are going to, or you have taken an overdose or you do not feel you can keep yourself or someone else safe.
You also have other options to get the help you need, so you can ring us, 111, the Samaritans, or attend A&E for a front door assessment, speak to a trusted friend or relative, your counsellor, your CPN, or if you are under the crisis team, ring the contact number, or if you need online advice there are additional resources available.
IGS: 999 ambulance Ring 999 IGS: Accident and emergency IGS: What to do in a crisis IGS: At risk of self-harm Ring 111 Ring Samaritans NHS: Urgent online help for mental healthPLEASE TAKE YOUR TIME
We realise everything may be very overwhelming and you don't know what to do or where to start. Please do take the time to read through our mental health resources page and perhaps, along with a trusted friend or relative, try and slowly work through the different sources of information in the required section. Not all of them will be applicable and you may need to try different things to help.
RING US IF YOU HAVE DIFFICULTIES
Do get in touch if you still have difficulties.
Ring usCITIZENS ADVICE BUREAU
Susan Tavassolian, GP Outreach Adviser from the Citizens Advice Bureau now writes about the service:
Outreach Appointments at Ivy Grove Surgery
Citizens Advice Derbyshire Districts holds advice sessions at Ivy Grove Surgery every Friday morning between 09:30am – 12:30pm. The appointments are for the patients of Ivy Grove Surgery and are by appointment only. Appointments can be booked by contacting the surgery – 01773 514130.
Citizens Advice Derbyshire Districts aims to provide a service that people need for the problems that they face. We aim to influence and improve policies and practices which affect people’s lives by providing statistical evidence to the decision makers.
Our service aims to provide information and advice upon a wide range of issues.
We provide free, independent, impartial and confidential advice to everyone on their rights and responsibilities. We value diversity, promote equality and challenge discrimination.
Free, Impartial, Confidential and Independent Advice
Welfare Benefits
We provide advice about benefit entitlement, the claiming process, help with the completion of benefit claims, both on paper and online and advise and assist with the appeal process.
Debt
We provide money and budgeting advice, this includes advising on the various options available, drawing up financial statements, negotiating with creditors and advising on court procedure including possession proceedings and completion of court forms.
Energy
We can assist with energy problems. This includes issues, with bills or meters, or if you are struggling to pay for the energy you use.
Employment
We can advise on employment issues which include employment rights, redundancy, dismissal and claims to an employment tribunal.
Housing
We can provide advice and negotiation on tenancy rights, homelessness and disrepair.
Family and relationship advice
We can provide advice and information regarding family and relationship issues such as divorce, separation, maintenance, child arrangements, death and bereavement.
Consumer problems
We can provide advice on credit, unsatisfactory goods and services, drafting letters and offering further negotiation.
Your appointment at Ivy Grove
To book an appointment with Citizens Advice, please speak to the reception team at Ivy Grove.
Following your initial appointment, if needed, follow up work and on-going casework can be undertaken on your behalf by a citizens advice caseworker and outside partnership organisations, if appropriate.
Susan Tavassolian
GP Outreach Adviser
DENTAL PROVISION
We are receiving lots of calls from many patients unhappy as a result of the increasing lack of dental provision, and asking us to treat them for their dental problem.
We urge all patients to ring their dentist (or 111 if not registered) if they have a dental need. In the same way that you would not ring your plumber to deal with an electrical problem, official guidance states that GPs should not deal with dental problems. Lack of appropriate dental provision does not mean this is then the responsibility of a GP.
This guidance has arisen as a result of patients having come to harm through being inappropriately or only partially treated by a GP, and whilst it may not feel like it, the guidance therefore exists to protect patients and keep them safe.
It is not common knowledge, but in the same way that doctors must offer same day urgent service where this is clinically appropriate, your dentist must also do the same, therefore please contact your dentist as you would normally if you have an emergency. Again lack of dental appointments, emergency or otherwise, does not make this an issue for your GP.
Your dentist can advise regarding problems within the mouth and can also refer you directly to hospital (or oral surgeon) where clinically necessary, as well as prescribe any pre-treatment and other necessary medications. We need to remind all our patients that it is practice policy that we do not prescribe diazepam (Valium) to sedate or calm any patient requiring dental work. Your dentist can advise (or prescribe) as needed.
In addition, it is dentists' responsibility to advise on anticoagulation (blood thinners) and whether these need to be continued or stopped prior to any dental work, based on the information that you provide to them about your medical condition(s). If it helps, we can provide you with a summary printout which you can show your dentist.
Finally, if you are not registered with a dentist, or cannot afford dental work, this does not mean that it then becomes the responsibility of a GP. Please ring 111 or go to the NHS website to find a local dentist who can treat you.
IGS: Dentist IGS: Diazepam policy for dentistry Ring 111 NHS: Find a local dentistDERMATOLOGY REFERRALS
In line with the move towards increased telemedicine, we have been notified that all dermatology referrals will now have to be made via an advice service incorporating photographs of any rash, lump or lesion so that the hospital can triage the request and advise us on any necessary action. We have been told that if photos are not supplied any such referral will be rejected.
We therefore encourage any patient who is looking to present to us with a skin lesion to be prepared to take photographs and to send them to us as part of any clinical assessment. If you need hints and tips on taking good photographs then please read the following guide:
Patient guide to taking better photosIf you need help responding to a text from the doctor asking you to send photos then please visit the following link:
AccuRx: My practice has asked me to respond to a text/send them a photo or documentNEW PRACTICE BUSINESS MANAGER
It’s time to welcome our new Practice Business Manager, Mr Ian Bonser, who joined us mid-August following the retirement of our previous practice manager, Charmagne. Here he introduces himself to you all:
Hi, my name is Ian, and I live in Mansfield with my wife and two young daughters.
I am delighted to have been offered the opportunity to join the team here at Ivy Grove Surgery as the Practice Business Manager, following Charmagne’s well-earned retirement.
In the relatively short time I have been here, I have been impressed with not only the work ethic and professionalism of the staff, but also how they ensure that the patient is always at the centre of everything they do.
I originally joined the NHS in 2017 when I retired from the RAF, after serving for 16 years. My previous NHS experience includes managing a similar sized surgery in Nottingham City, as well as working across secondary care and also with a primary care network.
My role here at the surgery is as varied as it gets! But in the main it involves; managing and coordinating all aspects of practice functionality, motivating and managing staff, optimising efficiency and financial performance and ensuring that the practice achieves its long-term strategic objectives in a safe and effective working environment.
I also oversee quality and continuous improvement, confidentiality, collaborative working, service delivery, learning and development and ensure that the practice complies with CQC regulations.
Please feel free to say hello, I look forward to meeting you all over the coming months and remember we love hearing about what we are doing well as well as what you feel we can improve on.
- Ian
NEW RECEPTION MANAGER
Debbie, our former reception manager, retired after 31 years at Ivy Grove Surgery. Here, our new reception manager, Louise, introduces herself:
Hi, my name is Louise, I am originally from Ripley and moved back 10 years ago. I have 6 children who keep me very busy, family is very important to me. I joined Ivy Grove in July replacing the lovely Debbie as Reception Team Leader.
My role within the practice involves a variety of administrative duties in line with patient care and also over seeing reception. No day is ever the same, as different challenges arise every day, but I love a good challenge!
I feel truly privileged to be given the opportunity to join the practice and work alongside such a lovely team, I am looking forward to meeting more of you and helping with any queries you may have.
- Louise
FLU CLINIC FEEDBACK
Ian now writes regarding the flu clinic which was held recently:
On Saturday October 8th, willing staff members (honestly!) from Ivy Grove Surgery, comprising of GPs and nurses as well as management and administrative staff gathered at the surgery for 7.30am, ready to begin the task of vaccinating the good patients of Ivy Grove Surgery, as our flu campaign got underway. Following bacon cobs and a quick drink, and a quick check that all of the clinical rooms were ready – the doors were opened, and we were up and running.
Whilst we will acknowledge at times that the wait was around 30 minutes (mainly due to us being a couple of vaccinators down on the day), luckily the weather was on our side and we managed to vaccinate just under 1800 patients between the hours of 8.00am and 3.00pm; which I think you will agree is pretty impressive number!
It was great to see the Ivy Grove team working so well together, in a slightly different setting to their normal day-to-day work. It was also nice for the staff to be able to chat to the patients, albeit briefly, as they moved along the queue. But it was particularly pleasing to see just how many patients showed their gratitude to the staff, for giving up their precious Saturday to ensure that as many of our patients as possible were offered protection against this year’s flu virus.
Those aged 50-64 years old, who are not in a clinical risk group, are also eligible this year, however, please note that this group will not be sent for until after all clinical at-risk patients have been given a chance to have a flu jab.
IGS: FluRECENT POSITIVE FEEDBACK
Continued thanks to all those patients who take the time to come back to us with heartwarming comments about the care they have received from the practice. These are all shared with our team and we really do appreciate each and every one of them, more so during these such difficult times. Thank you.
Having waited to queue for an appointment the receptionist was very kind helped me with a glass of water, booked me a telephone appointment (all l needed) to get some medication. After receiving a quick call back a prescription was sent immediately to my local chemist and collected within a very short time. Thank you to all at Ivy Grove - PH
Many thanks for the informative newsletter. I fully understand how pressurised you all are and thank you for all to do. Just one bit of feedback - when phoning the surgery, the same information is repeated a couple of times in the same call. Could the call process be shortened? It might lead to fewer irritable patients! With thanks -JM
I have just read the latest newsletter from Ivy Grove and would like to thank all the staff and doctors for their hard work and patience during these extremely busy times we all face. Abuse and violence is totally unacceptable to staff, doctors and other patients. The newsletter as always provides lots of useful information and new services available. Thank you to everyone – WB
I would like to thank whoever dealt with me on reception last week when I was so emotional. Your kindness was very much appreciated – MO
Dr Smith - Truly sorry that you are leaving. I'm still indebted to you for bothering to follow up my results, resulting in the early diagnosis and treatment of cancer. Wishing you and your family all the very best – AM
Dr Kamran, what a lovely, kind thorough doctor he is, an absolute credit to the surgery – HW
I wish to thank everyone for all their help. You always help me where ever you can – CF
Just wanted to say how kind Dr Francis was when he rang me on – JC
FINALLY...
Thank you for taking the time to read through yet another mammoth issue. Hopefully you will be more informed of the situation in General Practice and can act accordingly. We also sincerely hope that by the time of the next issue, we will have taken on some new doctors so that we can continue helping you, the good people of Ripley. Take care all of you.
Kind regards
Ivy Grove Surgery
Written by Dr M. Wong
© Dr Michael Wong 2022